They suggested that the pathoanatomy in these younger patients can complicate the surgery, the rehabilitation and the outcome of the shoulder arthroplasty. The preoperative diagnosis may have at least as much influence on the outcome of the procedure as does the age of the patient.
Recently, the authors of A History of Shoulder Instability is More Common in Young Patients Undergoing Total Shoulder Arthroplasty sought to evaluate whether a history of shoulder instability was more common in patients under 50 years old undergoing TSA. They identified 489 patients undergoing primary TSA within the Military Health System.
Patients under 50 years old were matched 1:2 with patients 50 years and older based on sex, race, and military status; the final study population comprised 240 patients.
The groups differed significantly in type of shoulder arthritis, with the older group having significantly more primary osteoarthritis (78% vs. 51%), while the younger group had significantly more patients with a history of shoulder instability (48% vs. 12%), prior ipsilateral shoulder surgery of any type (74% vs. 34%), and prior ipsilateral shoulder stabilization (31% vs. 5%). In the resultant logistic regression model, a history of shoulder instability (OR 5.0) and a history of any prior ipsilateral shoulder surgery (OR 3.5) were associated with TSA prior to the age of 50 years old.
Comment: From the foregoing, it is evident that the shoulder pathoanatomy of young patients having shoulder arthroplasty is different from that of older patients - a fact that may contribute to inferior results in these individuals after shoulder joint replacement.
Shoulder instability and its treatment can predispose the shoulder to arthritis observed in young patients. Below are some of the many reasons why this can happen.
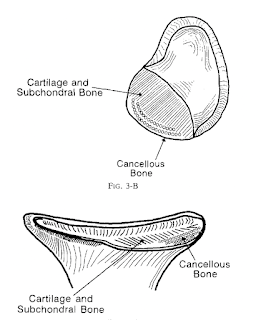
Recurrent instability can contribute to the development of glenohumeral arthritis from the forced translation of the humeral head over the lip of the glenoid can wear the articular cartilage
exposing the bone beneath
Surgery performed to manage instability can risk secondary arthritis from overtightening, leading to pathological translation and eccentric wear of cartilage (capsulorrhaphy arthropathy).
Prominent suture anchors used in instability surgery can lead to anchor arthropathy
Cutibacterium infection after instability surgery can lead to septic arthritis
In contrast to the situation with straightforward osteoarthritis, these conditions can complicate arthroplasty surgery and lead to suboptimal outcomes because of pathological alterations in bone and soft tissue quality and heightened risk of complications, such as periprosthetic infection.
Recognizing factors such as these can help patients and surgeons understand some of the differences in shoulder arthritis in younger patients and their effect on the success of joint replacement.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).