Primary glenohumeral osteoarthritis: clinical and radiographic classification. The Aequalis Group.
This often-quoted article forms the basis for what has become known as the Walch classification of pathoanatomy of the arthritic shoulder.
The authors obtained CT scans on 151 shoulders with primary osteoarthritis. They found that the average glenoid was retroverted and that posterior subluxation was present in almost half of the cases. They divided the radiographic appearance into type A without posterior erosion or displacement and type B with posterior erosion and/or displacement. They noted that posterior subluxation did not correlate with glenoid retroversion. Importantly, they make an observation overlooked by many surgeons: posterior instability is not necessarily resolved by normalizing glenoid version. They suggest that persistent posterior subluxation after total shoulder arthroplasty may give rise to what we have described as
'rocking horse' loosening of the glenoid component.
The categories of glenoid anatomy are shown in their diagram below.
This is very useful in showing some of the ends of the spectrum. It is apparent, however, there are many shades of grade between A1 and A2, between A1 and B1, between B1 and B2, between A2 and B2, and between B2 and C.
So, to show the 'shades of grade' issue, here are a few examples of what seem to be A1 glenoids.
First, minimal joint space narrowning
Next central thinning
Next anterior thinning
And next posterior thinning
Moving on to A2's, some appear on the borderline
While others are more obvious
Some A2's seem to border on B1's
And others show an anterior wear pattern, not part of the Walch classification.
Here are few B1's.
But some B1's border on B2's
Then there are the somewhat more obvious B2's
We reserve the "C" classification for glenoid dysplasia
All of this is to make two points: (1) CT scans are not necessary to determine glenoid pathology and (2) the categories as described in this article represent classic examples, but many shades exist between them. It is the classic issue of using categories to represent parametric variables, such as the degree of erosion or the posterior displacement of the head on the glenoid.
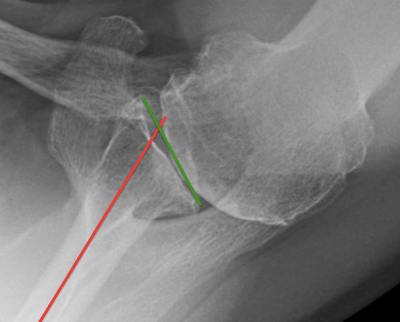
A final point. The authors propose a somewhat complex method for measuring the degree of subluxation:
where x-x' is a line parallel to the glenoid surface, y-y' is the perpendicular bisector of the articular segment of x-x' and z-z' is a line parallel to x-x' passing through the medial third of the humeral head. This method has the problem that slight alterations in the angle at which x-x' is drawn can have a substantial effect on the apparent anterior-posterior position of the head relative to the glenoid.
We are more interested in the degree to which the glenohumeral contact is centered on the glenoid.
A subsequent post will describe a simple method for quantitating the head position relative to the glenoid.
-------