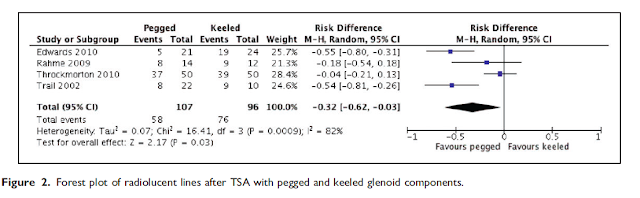
These authors conducted a systematic review of level I, II, and III studies comparing the development of radiolucent lines and glenoid failure after total shoulder arthroplasty with pegged or keeled glenoid components. Four articles were included in the final analysis with 107 pegged and 96 keeled glenoid components.
Development of radiolucent lines was less likely with pegged glenoid components with a risk difference of 0.32 (95% CI 0.62, 0.03) favoring the pegged design.
With the number of cases and the duration of followup in these studies, there was no statistically significant difference in the rate of radiographically at-risk glenoids, clinical glenoid failure, or the composite endpoint.
Comment: In considering the survivorship of glenoid components, it is important recognize that problems of glenoid component failure usually do not become evident until 5 or more years after the procedure. So comparative studies of revision rates for different components need to be extended well beyond the one year minimum applied in this study. Furthermore as evidenced in the study below, the rate of glenoid component failure is multifactorial.
Failure of the Glenoid Component in Anatomic Total Shoulder Arthroplasty
Although glenoid component failure is one of the most common complications of anatomic total shoulder arthroplasty, substantial evidence from the recent published literature is lacking regarding the temporal trend in the rate of this complication and the risk factors for its occurrence. We conducted a systematic review and identified twenty-seven articles presenting data on glenoid component failure rates that met the inclusion criteria. These articles represented data from 3853 total shoulder arthroplasties performed from 1976 to 2007. Asymptomatic radiolucent lines occurred at a rate of 7.3% per year after the primary shoulder replacement. Symptomatic glenoid loosening occurred at 1.2% per year, and surgical revision occurred at 0.8% per year. There was no significant evidence that the rate of symptomatic loosening has diminished over time. Keeled components had greater rates of asymptomatic radiolucent lines compared with pegged components in side-by-side comparison studies. However, as a result of wide variability in outcomes reporting, only sex, Walch class, and diagnosis were significantly associated with the risk of glenoid component failure in the overall analysis.
It is always of interest to review the data from the Australian NATIONAL JOINT REPLACEMENT REGISTRY (see this link), which demonstrates that an all polyethylene pegged glenoid component has a lower revision rate that keeled or metal backed components.
See also:
Rates of Radiolucency and Loosening After Total Shoulder Arthroplasty with Pegged or Keeled Glenoid Components
These results are consistent with what we published a decade ago, at which time we also factored in the importance of surgeon experience.
Finally, it is worth noting that all pegged components are not the same. Some have three smooth pegs in a row
=====
Rates of Radiolucency and Loosening After Total Shoulder Arthroplasty with Pegged or Keeled Glenoid Components
There is no question that survivorship of the glenoid component is the key to survivorship of a total shoulder arthroplasty. We have presented our approach to glenoid arthroplasty here.
This is an important study in that it seeks literature evidence on the cost-effectivenss of pegged vs. keeled glenoid components with particular emphasis on the risk of revision surgery. After a thorough analysis of the published data, they found that pooled risk ratio for revision was 0.27 (95% CI, 0.08 to 0.88) in favor of pegged components (p = 0.028). Their value analysis indicated that pegged glenoid designs were more cost-effective than keeled glenoid designs.
These results are consistent with what we published a decade ago, at which time we also factored in the importance of surgeon experience.
One of the key differences between a pegged and keeled component is that with a pegged component the geometry of the fit is more precisely controlled by the fact that concentric reaming takes place around the same axis as is used to fix the component.
Thus the risk of poor bony support for the component (shown below) is reduced.
Finally, it is worth noting that all pegged components are not the same. Some have three smooth pegs in a row
and others have out of plane peripheral pegs with a fluted central peg.
=====
The reader may also be interested in these posts:
Information about shoulder exercises can be found at this link.
Use the "Search" box to the right to find other topics of interest to you.
You may be interested in some of our most visited web pages including:shoulder arthritis, total shoulder, ream and run, reverse total shoulder, CTA arthroplasty, and rotator cuff surgery as well as the 'ream and run essentials'