These authors sought to compare the clinical and radiographic outcomes of augmented total shoulder arthroplasties (TSAs) vs. case-matched shoulders with standard implants to assess the early performance of a full-wedge augmented glenoid component.
Between 2010 and 2015, all TSAs using a full-wedge posteriorly augmented glenoid component with a minimum 2-year follow-up from a single institution were retrospectively reviewed. A total of 37 augmented TSAs were matched with 37 control shoulders with unaugmented glenoid components.
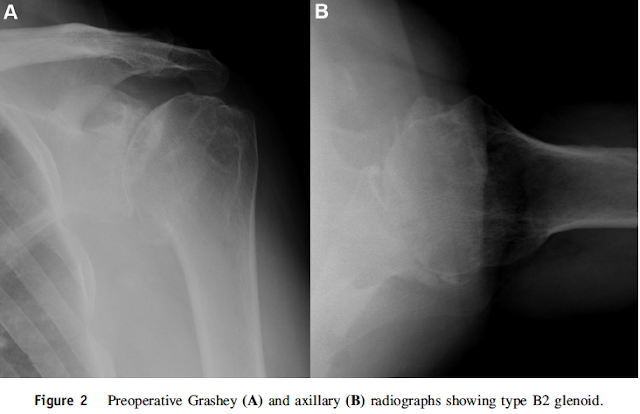
The article reports that both augmented and standard TSAs produced similar improvements in all ROM and PRO measures and that patients with augmented glenoid components were more likely to have type B2 or B3 deformities (P . .004).
At final follow-up, 54% of augmented glenoids showed implant lucencies compared with 46% of control shoulders. The mean Lazarus score remained similar between groups. When 8 and 16 degree augmentations were compared, the 16 degree augmentation demonstrated a significantly higher mean Lazarus score.
This article states that "Failure to correct glenoid version can result in persistent posterior subluxation and progressive glenoid loosening." But the Discussion points out that preoperative version and postoperative version were unable to be assessed. Early in the study period, CT imaging was not uniformly obtained...postoperative correction was unable to be assessed with CT scans, which we are unable to routinely obtain because of concerns of radiation and cost...institutional constraints on obtaining multiplanar imaging postoperatively."
Comment: In that the goal of the augmented glenoid is to "correct glenoid version", the article does not indicate whether this goal was achieved due to the absence of preoperative and postoperative version measurements.
It has been demonstrated that a standardized axillary view can yield measurements of version closely approximating those achieved with CT scans. This enables preoperative and postoperative comparisons without the concerns of"radiation and cost".
This article does not demonstrate advantages to the patient of correcting glenoid version using an augmented glenoid component. Such studies need to be considered in light of evidence that it may not be necessary to "correct" retroversion as demonstrated in the article below.
Does Postoperative Glenoid Retroversion Affect the 2-Year Clinical and Radiographic Outcomes for Total Shoulder Arthroplasty?
While glenoid retroversion and posterior humeral head decentering are common preoperative features of severely arthritic glenohumeral joints, the relationship of postoperative glenoid component retroversion to the clinical results of total shoulder arthroplasty (TSA) is unclear. Studies have indicated concern for inferior outcomes when glenoid components are inserted in 15° or more retroversion.
In a population of patients undergoing TSA in whom no specific efforts were made to change the version of the glenoid, these authors asked whether at 2 years after surgery patients having glenoid components implanted in 15° or greater retroversion had (1) less improvement in the Simple Shoulder Test (SST) score and lower SST scores; (2) higher percentages of central peg lucency, higher Lazarus radiolucency grades, higher mean percentages of posterior decentering, and more frequent central peg perforation; or (3) a greater percentage having revision for glenoid component failure compared with patients with glenoid components implanted in less than 15° retroversion. They examined the records of 201 TSAs performed using a standard all-polyethylene pegged glenoid component
The mean (± SD) improvement in the SST (6.7 ± 3.6; from 2.6 ± 2.6 to 9.3 ± 2.9) for the retroverted group was not inferior to that for the nonretroverted group (5.8 ± 3.6; from 3.7 ± 2.5 to 9.4 ± 3.0). The percent of maximal possible improvement (%MPI) for the retroverted glenoids (70% ± 31%) was not inferior to that for the nonretroverted glenoids (67% ± 44%). The 2-year SST scores for the retroverted (9.3 ± 2.9) and the nonretroverted glenoid groups (9.4 ± 3.0) were similar (mean difference, 0.2; 95% CI, - 1.1 to 1.4; p = 0.697). No patient in either group reported symptoms of subluxation or dislocation. The radiographic results for the retroverted glenoid group were similar to those for the nonretroverted group with respect to central peg lucency (four of 21 [19%] versus six of 50 [12%]; p = 0.436; odds ratio, 1.7; 95% CI, 0.4-6.9), average Lazarus radiolucency scores (0.5 versus 0.7, Mann-Whitney U p value = 0.873; Wilcoxon rank sum test W = 512, p value = 0.836), and the mean percentage of posterior humeral head decentering (3.4% ± 5.5% versus 1.6% ± 6.0%; p = 0.223). The percentage of patients with retroverted glenoids undergoing revision (0 of 21 [0%]) was not inferior to the percentage of those with nonretroverted glenoids (three of 50; [6%]; p = 0.251).
These authors concluded that in this series of TSAs, postoperative glenoid retroversion was not associated with inferior clinical results at 2 years after surgery.
While glenoid retroversion and posterior humeral head decentering are common preoperative features of severely arthritic glenohumeral joints, the relationship of postoperative glenoid component retroversion to the clinical results of total shoulder arthroplasty (TSA) is unclear. Studies have indicated concern for inferior outcomes when glenoid components are inserted in 15° or more retroversion.
In a population of patients undergoing TSA in whom no specific efforts were made to change the version of the glenoid, these authors asked whether at 2 years after surgery patients having glenoid components implanted in 15° or greater retroversion had (1) less improvement in the Simple Shoulder Test (SST) score and lower SST scores; (2) higher percentages of central peg lucency, higher Lazarus radiolucency grades, higher mean percentages of posterior decentering, and more frequent central peg perforation; or (3) a greater percentage having revision for glenoid component failure compared with patients with glenoid components implanted in less than 15° retroversion. They examined the records of 201 TSAs performed using a standard all-polyethylene pegged glenoid component
inserted after conservative glenoid reaming without specific attempt to modify preoperative glenoid version.
Of these, 171 (85%) patients had SST scores preoperatively and between 18 and 36 months after surgery. Ninety-three of these patients had preoperative radiographs in the database and immediate postoperative radiographs and postoperative radiographs taken in a range of 18 to 30 months after surgery. Twenty-two patients had radiographs that were inadequate for measurement at the preoperative, immediate postoperative, or latest followup time so that they could not be included. In comparison to those included in the analysis, the excluded patients did not have substantially different mean age, sex distribution, time of followup, distribution of diagnoses, American Society of Anesthesiologists class, alcohol use, smoking history, BMI, history of prior surgery or preoperative glenoid version. They analyzed the two year outcomes in the remaining 71 TSAs, comparing the 21 in the retroverted group (the glenoid component was implanted in 15° or greater retroversion (mean ± SD, 20.7° ± 5.3°)) with the 50 in the non-retroverted group ( the glenoid component was implanted in less than 15° retroversion (mean ± SD, 5.7° ± 6.9°)).
The mean (± SD) improvement in the SST (6.7 ± 3.6; from 2.6 ± 2.6 to 9.3 ± 2.9) for the retroverted group was not inferior to that for the nonretroverted group (5.8 ± 3.6; from 3.7 ± 2.5 to 9.4 ± 3.0). The percent of maximal possible improvement (%MPI) for the retroverted glenoids (70% ± 31%) was not inferior to that for the nonretroverted glenoids (67% ± 44%). The 2-year SST scores for the retroverted (9.3 ± 2.9) and the nonretroverted glenoid groups (9.4 ± 3.0) were similar (mean difference, 0.2; 95% CI, - 1.1 to 1.4; p = 0.697). No patient in either group reported symptoms of subluxation or dislocation. The radiographic results for the retroverted glenoid group were similar to those for the nonretroverted group with respect to central peg lucency (four of 21 [19%] versus six of 50 [12%]; p = 0.436; odds ratio, 1.7; 95% CI, 0.4-6.9), average Lazarus radiolucency scores (0.5 versus 0.7, Mann-Whitney U p value = 0.873; Wilcoxon rank sum test W = 512, p value = 0.836), and the mean percentage of posterior humeral head decentering (3.4% ± 5.5% versus 1.6% ± 6.0%; p = 0.223). The percentage of patients with retroverted glenoids undergoing revision (0 of 21 [0%]) was not inferior to the percentage of those with nonretroverted glenoids (three of 50; [6%]; p = 0.251).
These authors concluded that in this series of TSAs, postoperative glenoid retroversion was not associated with inferior clinical results at 2 years after surgery.
===
We have a new set of shoulder youtubes about the shoulder, check them out at this link.
Be sure to visit "Ream and Run - the state of the art" regarding this radically conservative approach to shoulder arthritis at this link and this link
Use the "Search" box to the right to find other topics of interest to you.
You may be interested in some of our most visited web pages arthritis, total shoulder, ream and run, reverse total shoulder, CTA arthroplasty, and rotator cuff surgery as well as the 'ream and run essentials'