Failure of the subscapularis after shoulder arthroplasty is a clinically important complication that can substantially compromise the comfort and function of the shoulder.
Take down and repair
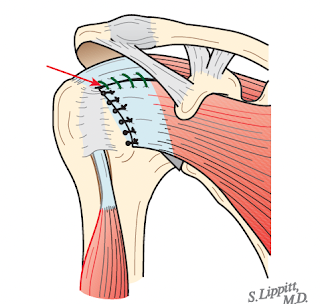
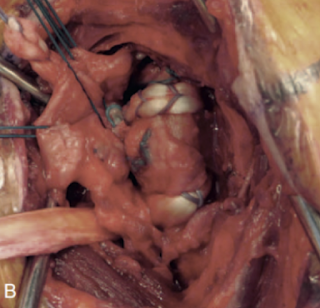
Like most complications, subscapularis failure is better prevented than treated. Our approach includes takedown using a careful subscapularis peel, keeping the subjacent capsule intact to the tendon.
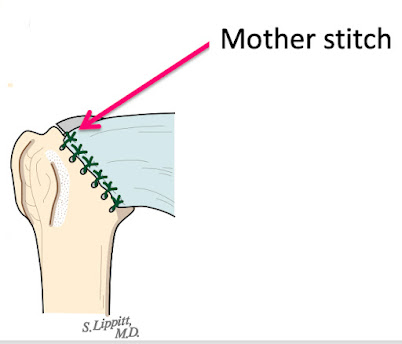
After the arthroplasty, the subscapularis tendon and subjacent capsule are repaired to the humerus using at least 6 sutures passed through secure drill holes at the margin of the humeral head cut.
This repair can be reinforced with a rotator interval plication.
Diagnosing failure
Because post operative MRIs and sonograms after shoulder arthroplasty can be difficult to interpret, the diagnosis of subscapularis failure is often best made from
(1) history - force on the repaired tendon within the first two months after surgery resulting from
a fall on the arm,
a sudden or unexpected stretch in external rotation beyond the handshake position
a forceful internal rotation (e.g. while restraining a dog chasing a squirrel)
(2) physical exam
increased external rotation from what was recorded in the operating room at the close of the case
They conducted a retrospective study of patients who underwent primary anatomic TSA with subscapularis tenotomy using either transosseous repair (TOR #=192) or direct primary tendon repair (PTR #=114) of a subscapularis tenotomy.
The "primary outcome studied was clinical subscapularis failure, defined as anterior subluxation of the glenohumeral joint as seen on axillary lateral radiographs with accompanying clinical decompensation, including pain and loss of active forward elevation and internal rotation.""Patients were not routinely screened by ultrasound or MRI to evaluate subscapularis integrity. Additionally, internal rotation strength testing was based on manual muscle testing. Clinical assessment of internal rotation strength is fairly subjective and limited because nearly all of the patients had 4/5 or 5/5 internal rotation strength." Substantial emphasis was placed on the patient's response to a question from the ASES score which asks about the ability to perform functional internal rotation activities such as putting on a bra or washing the back. Of note only 41.4% of the TOR group and 33.3% of the PTR group responded with “not difficult.”
Subscapularis failure was recognized in 13 patients (4.2% among the TOR group and 4.4% among the PTR group). Reoperation was performed in 18 patients. Subscapularis failures, complications not requiring surgery, and reoperations were not significantly different between the two groups.
Comment: In this retrospective study of an institutional database it appears that the patients in this series may not have been routinely and systematically examined for subscapularis failure, but rather the diagnosis was inferred from radiographs and from ASES scores. It is therefore possible that the rate of subscapularis failure was underestimated.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
How you can support research in shoulder surgery Click on this link.
Here are some videos that are of shoulder interest