Here are a few recent articles that may be of interest.
Prevention
Does preoperative corticosteroid injection increase the risk of periprosthetic joint infection after reverse shoulder arthroplasty? reported a significantly increased risk of PJI in patients who received corticosteroid injections (CJI) within 1 month of reverse total shoulder, but not those who received CSI more than 1 month before RSA. Alcohol abuse, chronic kidney disease, and depression were also identified as factors increasing the risk of PJI.
Photodynamic therapy for Cutibacterium acnes decolonization of the shoulder dermis found that the use of photodynamic therapy did not significantly reduce dermal colonization of Cutibacterium (as determined by punch biopsy cultures) as compared to standard skin preparation. The overall positive culture rate was 54%. All positive cultures identified Cutibacterium except for one.
Effect of Making Skin Incision with Electrocautery on Positive Cutibacterium acnes Culture Rates in Shoulder Arthroplasty: A Prospective Randomized Clinical Trial discovered that cultures obtained from the incised dermal edge immediately after skin incision were less likely to be positive if electrocautery was used in making the skin incision. However, there was no significant difference in the positive culture rate in samples from gloves and forceps taken immediately prior to humeral component implantation. Thus, use of cautery did not reduce the rate of wound innoculation.
Diagnosis
The Incidence of Subclinical Infection in Patients Undergoing Revision Shoulder Stabilization Surgery: A Retrospective Chart Review twenty-nine (27%) of 107 patients having revision surgery had positive cultures. Twenty-six patients had positive Cutibacterium cultures; these cultures took an average of 10.65 days to turn positive. The authors suggest that surgeons consider infection as a reason for lack of clinical improvement and possibly needing revision surgery after shoulder stabilization.
In The role of sonication in the diagnosis of periprosthetic joint infection in total shoulder arthroplasty the standard synovial fluid cultures combined with intraoperative periprosthetic tissue cultures had a sensitivity of 95%, specificity of 95% and total accuracy of 95%. Sonication cultures had a sensitivity of 91%, specificity of 68% and total accuracy of 80%.
Treatment
Outcomes after Debridement, Antibiotics, and Implant Retention for Prosthetic Joint Infection in Shoulder Arthroplasty found that 29.4% of thee patients were diagnosed as having recurrent infection on chart review.
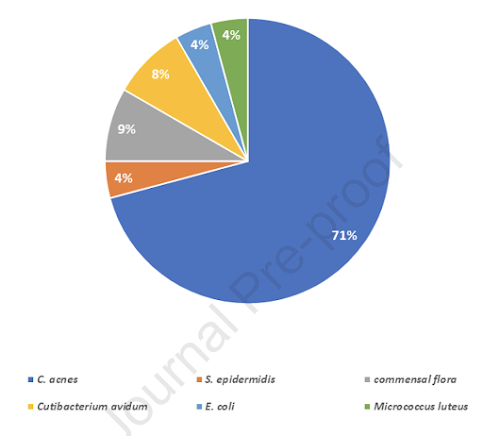
High infection control rate after systematic one-stage procedure for shoulder arthroplasty chronic infection found that 36/40 patients had no recurrence of infection after the one stage revision. Cutibacterium was the most frequent pathogen isolated, found in 67.5% (27/40) of the patients. The infection was polymicrobial in 40% (16/40) of the cases.
One-stage revision for infected shoulder arthroplasty: prospective, observational study of 37 patients found that 95% did not have evidence of recurrent infection. The most commonly isolated pathogen was Cutibacterium acnes (68%), isolated alone (15 patients, 41%) or as polymicrobial infections (10 patients, 27%).
Outcomes after resection arthroplasty versus permanent antibiotic spacer for salvage treatment of shoulder periprosthetic joint infections: a systematic review and meta-analysis found that when implant exchange after shoulder PJI is not feasible, permanent antibiotic spacers and resection arthroplasty are both salvage procedures that provide similar rates of infection eradication. Although both can decrease pain levels, the permanent antibiotic spacer may result in better functional outcomes compared with resection arthroplasty.
Comment: It is apparent that the experience in the diagnosis and treatment hip and knee PJI cannot be directly applied to the shoulder because of the difference in causative bacteria.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).