These authors conducted a retrospective review of the minimum 2 year outcomes for 189 primary total shoulder arthroplasty patients having a lesser tuberosity osteotomy (LTO) to take down the subscapularis.
The LTO was repaired using a series of 4 transosseous FiberWire sutures placed through the biceps groove with an additional FiberTape suture placed as a cerclage suture through the greater tuberosity, wrapped around the humeral stem, and passed through the bone tendon junction of the subscapularis.
Postoperatively, patients wore a shoulder immobilizer with pendulum exercises only for the first 6 weeks, followed by an active-assisted stretching program. Strengthening and lifting were delayed for 3 months.
Three patients were treated with revision. One patient with a displaced LTO nonunion did not improve clinically and was converted to a reverse shoulder arthroplasty. One patient developed a late postoperative infection at 5 years and was treated with a 2-stage revision to a reverse shoulder arthroplasty. The other developed a massive rotator cuff tear of the supraspinatus and infraspinatus 5 years after surgery and was revised to a reverse shoulder arthroplasty.
Comment: This is an interesting study that shows the importance of secure subscapularis reattachment after shoulder arthroplasty and the results of LTO in expert hands. The article points to the need for care during the first 3 months after repair, avoiding active internal rotation and passive stretching in external rotation.
Postoperatively, patients wore a shoulder immobilizer with pendulum exercises only for the first 6 weeks, followed by an active-assisted stretching program. Strengthening and lifting were delayed for 3 months.
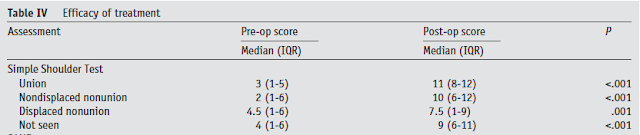
Postoperative radiographs were used to classify LTO healing as “bony union,” “nondisplaced nonunion,” “displaced nonunion,” and “not seen.”
24% of patients did not have radiographic union: 16 had nondisplaced nonunion, 14 had displaced nonunion, and in 16 the lesser tuberosity was not seen.
An example of a displaced non union is shown below.
Patients with displaced nonunions had
(1) no improvement in Single Assessment Numeric Evaluation or internal rotation,
(2) lower postoperative Simple Shoulder Test scores
(3) higher pain scores and
(4) a higher rate of glenoid gross loosening.
Three patients were treated with revision. One patient with a displaced LTO nonunion did not improve clinically and was converted to a reverse shoulder arthroplasty. One patient developed a late postoperative infection at 5 years and was treated with a 2-stage revision to a reverse shoulder arthroplasty. The other developed a massive rotator cuff tear of the supraspinatus and infraspinatus 5 years after surgery and was revised to a reverse shoulder arthroplasty.
Instead of an LTO, we prefer a careful subscapularis peel and reattachment for several reasons:
(1) it does not require sacrifice of the biceps tendon
(2) it does not compromise the strength of the proximal humerus
(3) it does not require the complex suture / tape technique described above
(4) by leaving the capsule on the deep surface of the tendon, repair sutures can be securely passed through tissue of good quality on both the tendon side and the bone side
=====
We have a new set of shoulder youtubes about the shoulder, check them out at this link.
Use the "Search" box to the right to find other topics of interest to you.
You may be interested in some of our most visited web pages arthritis, total shoulder, ream and run, reverse total shoulder, CTA arthroplasty, and rotator cuff surgery as well as the 'ream and run essentials'