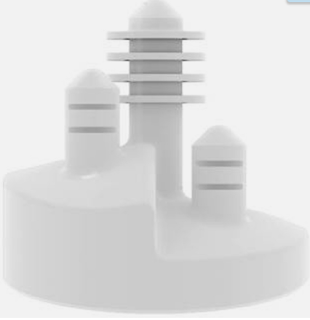
In their classic article, Stepped Augmented Glenoid Component in Anatomic Total Shoulder Arthroplasty for B2 and B3 Glenoid Pathology, the authors demonstrate that a stepped augmented glenoid component can restore premorbid glenoid anatomy in patients with asymmetric biconcave glenoid bone loss (Walch B2), with short-term clinical and radiographic results equivalent to those for patients without glenoid bone loss (Walch A1) treated with a non-augmented component.
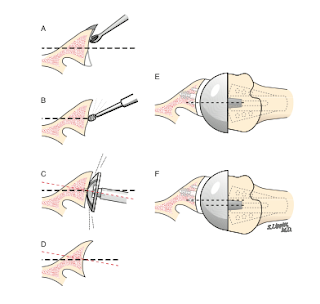
They found a greater risk of osteolysis around the central peg in patients with moderate-to-severe B3 glenoid pathology with this stepped augmented glenoid component. As demonstrated in the technique guide, use of this component involves reaming of the posterior glenoid to fit the step, which may diminish the bony support for the back of the component.
Should this component fail, the posterior bone stock available for conversion to a reverse total shoulder may be compromised.
A recent paper, Total Shoulder Arthroplasty for Glenohumeral Arthritis Associated with Posterior Glenoid Bone Loss: Midterm Results of an All-Polyethylene, Posteriorly Augmented, Stepped Glenoid Component, presented a 5 year followup of 35 shoulders receiving a stepped glenoid for the treatment of glenohumeral osteoarthritis with posterior glenoid bone loss. The average preoperative glenoid retroversion was 21.6˚. Although postoperative CT scans were obtained, the postoperative glenoid retroversion was not presented.
Two patients (6%) experienced prosthetic instability requiring revision.
The average Lazarus score (0 no radiolucency to 5 gross loosening) was 0.72. The average Yian score (0 no radiolucency to 18 radiolucent line around entire component) was 2.6. There was an increase in Lazarus score and decrease in Wirth score between 2- and 5-year follow-up. The severity of radiographic loosening correlated with patient-reported pain levels.
The authors point out that these results are not inferior to those achieved with standard glenoid components in the treatment of glenohumeral arthritis with posterior bone loss.
Comment: Since posterior reaming removes posterior bone and the stepped component adds posterior polyethylene, it would be of interest to know the net change in glenoid retroversion in these patients.
Two figures from this series seem to suggest that substantial retroversion remains after insertion of the stepped component.
As pointed out in the two posts referenced below, future research is needed to determine the clinical value and means of "correcting" glenoid retroversion.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).