Subluxation of a joint is defined by the World Health Organization as an "incomplete or partial dislocation"
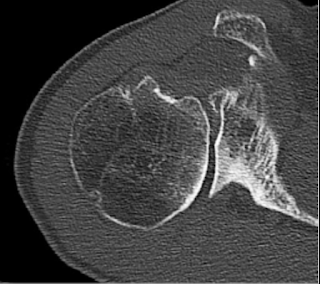
Posterior subluxation of the humeral head on the glenoid is shown below in an axillary view taken with the arm in a position of functional elevation. Because it loads the back of the shoulder, this "truth" view may be better at detecting posterior decentering than a CT taken with the arm at the side. See Answering the critical question: "To what degree is the humeral head functionally centered on the glenoid?" in 6 easy steps.

See Functional malcentering of the humeral head and asymmetric long-term stress on the glenoid: Potential reasons for glenoid loosening in total shoulder arthroplasty ("we found that only 25% of the patients demonstrated a fixed posterior malcentering in a relaxed situation, but 85% showed a functional de-centering during elevation of the arm").
The topic of arthritic shoulder subluxation is obviously of great interest in that the number of articles relating to it is increasing each year.

The amount of posterior subluxation of the humeral head on the glenoid can be determined on an axillary projection as described by Walch et al in Primary glenohumeral osteoarthritis: clinical and radiographic classification. The Aequalis Group
Another approach uses the scapular body - rather than the glenoid articular surface - as the reference. In this method a line is drawn from the tip of the medial border of the scapula to the center of the glenoid fossa; the degree of subluxation is defined as the amount of humeral head lying posterior to this line. As shown in the figure below modified from Approach to glenoid bone loss and deformity in B3 and C glenoids: Primary anatomic shoulder arthroplasty, this method will show a substantial amount of "subluxation" in B3 and C glenoids.
However, applying the original Walch method to this example finds that the humeral head is centered in the glenoid (i.e. not subluxated).
However the relationship of the humeral head to the plane of the scapula does not reveal the degree of centering or decentering of the humeral head in the glenoid. This helps us understand that the difference between an A2 glenoid and a B3 glenoid lies not in the degree to which the humeral head is centered in the glenoid, but rather in the degree of retroversion
Similarly, the humeral head is often centered on the retroverted type C glenoid.
Version can be altered using eccentric reaming, posterior bone graft or augmented glenoid components - each of which may add complexity, cost, and complications.
Thus, in the treatment of symptomatic B3 and C glenoids, the surgeon needs to decide if altering glenoid version is worthwhile. See Glenoid version: acceptors and correctors
The authors of Early to midterm outcomes of anatomic shoulder arthroplasty performed on dysplastic glenoids studied 29 patients with Type C glenoids with minimum 2 year follow-up after anatomic total shoulders with standard components compared to a matched cohort of 58 A1 glenoids. No effort was made to correct glenoid version through reaming or posterior bone graft. They found similar outcomes scores, patient satisfaction, complication rates, and revision rates.
Treatment of posterior decentering is a different matter and can usually be accomplished without changing glenoid version as demonstrated in Management of intraoperative posterior decentering in shoulder arthroplasty using anteriorly eccentric humeral head components
A more extensive review of subluxation and its clinical importance can be found in Subluxation in the Arthritic Shoulder The authors critically reviewed the use and misuse of the term "subluxation" in the characterization of arthritic shoulders. Their bullet points are listed below:
» The term “subluxation” means partial separation of the joint surfaces. In the arthritic shoulder, “arthritic glenohumeral subluxation” refers to displacement of the humeral head on the surface of the glenoid.
» The degree of arthritic glenohumeral subluxation can be measured using radiography with standardized axillary views or computed tomography (CT).
» Shoulders with a type-B1 or B2 glenoid may show more posterior subluxation on an axillary radiograph that is made with the arm in an elevated position than on a CT scan that is made with the arm at the side.
» The degree of arthritic glenohumeral subluxation is not closely related to glenoid retroversion.
» The position of the humeral head with respect to the plane of the scapula is related to glenoid retroversion and is not a measure of glenohumeral subluxation.
» Studies measuring glenohumeral subluxation before and after arthroplasty should clarify its importance to the clinical outcomes of shoulder reconstruction.
Applying the standard definition, "subluxation" refers to the displacement of the humeral head relative to the glenoid articular surface. In the diagram below, posterior displacement of the center of a circle that is fit to the humeral head articular surface (decentering) is shown with respect to the perpendicular bisector (red line) of a line segment connecting the anterior and posterior edges of the glenoid. The amount of displacement (the length of the line segment with double arrows) can be expressed as a percentage of the diameter of the circle.

The figure below shows the posterior displacement of the center of a circle fit to the humeral head articular surface with respect to the scapular body reference (long blue line). The amount of displacement (the length of the line segment with double arrows) can be expressed as a percentage of the diameter of the circle. Displacement of the humeral head relative to the plane of the scapular body is not the same as subluxation in that it does not indicate the degree of displacement of the joint surfaces.
As shown in the diagram below, the degree of posterior subluxation ( decentering) of the humeral head realative to the glenoid (red symbols) for the different glenoid types is not related to the amount of glenoid retroversion. On the other hand the degree of posterior displacement of the humeral head relative to the scapular body (blue symbols) for the different glenoid types is essentially linearly related to the amount of glenoid retroversion.

The amount of posterior subluxation of the humeral head relative to the glenoid is affected by the position of the arm when the image is made. In the graph below, note that the amount of posterior decentering for shoulders with B1 and B2 glenoids is greater for axillary views taken with the arm in a position of functional elevation (blue symbols, see x-ray at the top of this post) in comparison to that for CT scans taken with the arm positioned at the side (red symbols). Note also that the A1, A2 and B3 glenoids remain centered in both arm positions.

Comment: The measurement of subluxation of the humeral head in relation to the glenoid is an important element in understanding and managing the arthritic shoulder. The different glenoid types show characteristic patterns of glenohumeral subluxation that are not closely related to the degree of glenoid retroversion. The relationship of the humeral head to the body of the scapula is mostly related to glenoid retroversion and is not a measure of glenohumeral subluxation.
Consistency and appropriate use of the term “subluxation” will enhance our understanding of arthritic glenohumeral pathoanatomy and its management.
Use of the same imaging technique and arm position before and after surgery enables the surgeon to evaluate the effectiveness of arthroplasty in re-centering the humeral head on the glenoid
Thanks to Mihir Sheth, UW shoulder fellow, for his help in preparing this post.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter (X): https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).