Short stem humeral implants have been introduced to the market based on the proposition that they are "bone preserving". One might ask:
Do they require less bone removal than a standard stemmed implant?
Do they result in less stress shielding and adaptive bone loss than a standard stemmed implant?
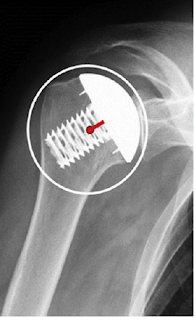
Because short stems achieve fixation through a snug fit of the prosthesis in the proximal humerus, stress shielding is commonly observed (see
Radiographic changes differ between two different short press-fit humeral stem designs in total shoulder arthroplasty and
Postoperative radiographic findings of an uncemented convertible short stem for anatomic and reverse shoulder arthroplasty and
Radiologic bone adaptations on a cementless short-stem shoulder prosthesis).
The challenge with short stems is to achieve fixation without stress shielding. See examples of stress shielding with short stemmed components below.
The authors of The effect of humeral implant thickness and canal fill on interface contact and bone stresses in the proximal humerus studied the effects of implant thickness and canal fill on load transfer, contact, and stress shielding in a finite element study comparing three generic short-stem implant models with different cross-sectional thickness (thinner ( 8 mm), medium (12 mm), and thicker (16 mm).
They determined (1) the amount of bone-to-implant contact, (2) changes in cortical and trabecular bone stresses from the intact state, and (3) changes in cortical and trabecular strain energy densities which can predict bone remodeling or stress shielding.
They found that the thinner implant with the lowest canal fill ratio produced significantly lower changes in stress from the intact state in both cortical and trabecular bone. In addition, the thinner implant resulted in a substantially lower volume of bone predicted to stress shield and resorb when compared with the medium and thicker stems.
They concluded that thinner implants and lower canal fill may be beneficial over thicker sizes, provided equal initial fixation can be achieved. The thinner implant has a greater degree of load sharing and increases the mechanical load placed on surrounding bone, reducing the risk of stress shielding and bone resorption.
The question becomes "how is fixation of a thin stem achieved?". Furthermore, if a thin stem is used, what is the advantage of a short stem? The amount of bone removed is the same for both as pointed out in Anatomic short-stem humeral component in total shoulder arthroplasty: a retrospective analysis.


With a standard length stem, impaction autografting can be used to achieve secure fixation of a thin stem on one hand and avoid problems with stress shielding on the other.
The authors of Radiographic outcomes of impaction-grafted standard-length humeral components in total shoulder and ream-and-run arthroplasty: is stress shielding an issue? evaluated humeral stress shielding after shoulder arthroplasty performed with a smooth, standard-length humeral stem fixed with impaction autografting.
Prior to placement of the final component, cancellous autograft harvested from the humeral head was placed in the humeral canal and pressed into place using a humeral impactor with the same stem geometry as the implant. Autograft was progressively inserted until the impactor fit tightly within the humerus. The final uncoated, smooth, stemmed, fixed-angle humeral component with the desired head geometry was then driven into the prepared canal.
At two years after surgery, the radiographic appearances were evaluated by an independent experienced shoulder surgeon from another institution not involved in the care of these patients. The metaphysical and diaphysial filling ratios were measured as shown below.
The filling ratios were small, showing a substantial preservation of bone stock.
The overall radiographic results are shown below
These authors concluded that the independent assessment of the 2-year radiographic and clinical outcomes of a conventional smooth humeral stem inserted with impaction autografting demonstrated the clinical utility of this bone-preserving approach to humeral component fixation with minimal complications; good clinical outcomes; and low rates of bone loss, component subsidence, and shift in position.
Impaction allografting is a useful method for addressing failed prior short stem humeral component fixation - no additional bone is removed


Symptomatic Aseptic Loosening of a Short Humeral Stem Following Anatomic Total Shoulder Arthroplasty
These authors point out that the rate of aseptic humeral component loosening with standard-length stems is low (0.3%) and that presence of humeral loosening gives rise to concern for periprosthetic shoulder infection.
They conducted a retrospective multi-institutional review of anatomic total shoulders performed with a grit-blasted, rectangular short humeral stem without ingrowth coating.
Twenty-three (12.5%) patients presented with a painful shoulder and met the authors' criteria for humeral loosening at a mean follow-up of 1.5 years (range: 1.5 months – 3.4 years); half had gross humeral subsidence. Thirteen (7.1%) of these underwent revision shoulder arthroplasty where a loose stem was confirmed.
The rate of symptomatic aseptic humeral loosening in this series was 10.9% (20/184) with 5.4% undergoing revision surgery. Patients with symptomatic aseptic humeral loosening were more likely to be male (90.5%) than those patients without symptoms (52.8%; p<0.001). Of the 105 male shoulders included in this cohort, 19 (18.0%; 19/105) developed symptoms and radiographic findings concerning for aseptic loosening. Ten (9.5%; 10/105) had a revision for aseptic loosening.
The authors concluded that the early humeral loosening rate for this stem design "far outpaces previously reported rates and this study likely under-reports the true incidence of clinically-significant loosening as it only contains limited short-term follow-up".
Comment: Based on the above information, short stemmed humeral components do not provide added value in comparison to impaction autografted thinner standard length humeral stems.