These authors reviewed 47 patients having revision for periprosthetic infections of the shoulder: 27 underwent a 2-stage revision, and 20 were treated with an antibiotic spacer as definitive treatment.
A recurrent infection was recognized in 3 patients in the antibiotic spacer group and 2 patients in the 2-stage revision group.
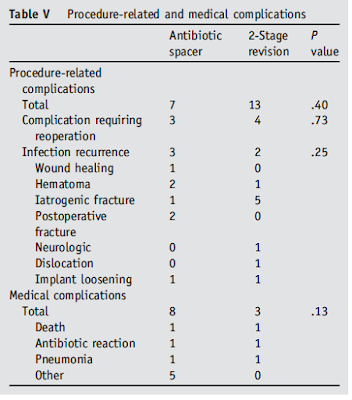
A total of 20 procedure-related complications (43%) and 11 medical complications (23%) occurred among the 47 patients. All 3 reoperations in the spacer group were due to recurrent infections. Of the 4 reoperations in the 2-stage group, 2 were due to recurrent infections; the other reoperations were due to a woundhealing complication and humeral stem loosening after reimplantation of the final shoulder arthroplasty. Adverse reactions to IV vancomycin developed in 1 patient from each study group. In the patient in the 2-stage group, Stevens-Johnson syndrome developed, requiring admission to the hospital. In the other patient, an allergic response to the medication developed after 2 weeks of treatment, requiring a change in medication. Additional complications in the spacer group included deep vein thrombosis, myocardial infarction, hip fracture, acute renal failure, and a suicide attempt from an opioid overdose. Two deaths occurred within the first year of surgery. One death occurred as a result of a suicide approximately 9 months after the second-stage reimplantation. The other death occurred owing to sepsis from pneumonia; the patient had undergone antibiotic spacer placement approximately 5 months earlier.
Comment: This article points to the high complication rate associated with surgery in managing an infected shoulder arthroplasty. Of interest, 38% of the patients planned for a two-stage revision refused to proceed with the second stage.
This paper did not distinguish the treatment and outcomes of low virulence organisms (Cutibacterium and coagulase negative Staph (CoNS)), from those with high virulence organisms (Staph aureus and gram negatives). As pointed out in the article below, we have found that periprosthetic infections with Cutibacterium can be satisfactorily treated with a single stage revision - a safer procedure than using a spacer and a two-stage revision. We suggest that future studies should evaluate the management of periprosthetic infections from Cutibacterium and CoNS separately from the management of more virulent organisms.
Single-Stage Revision Is Effective for Failed Shoulder Arthroplasty with Positive Cultures for Propionibacterium
Fifty-five shoulders without obvious clinical evidence of infection had a single-stage revision arthroplasty. Specifically all components (humeral and glenoid) were removed, a thorough debridement was carried out and a new humeral hemiarthroplasty was inserted with Vancomycin impregnated allograft. The residual glenoid bone was smoothed, but not bone grafted. No glenoid components were replaced.
Preoperative antibiotics were withheld until culture specimens were taken; a minimum of 5 tissue or explant specimens were obtained from each shoulder. Specimens were cultured for 21 days on blood agar (trypticase soy agar with 5% sheep blood), chocolate agar, Brucella agar (with blood, hemin, and vitamin K), and brain-heart infusion broth. Bacteria that were isolated received a full species-level identification by means of 16S rDNA sequencing.
The culture-positive group were 89% male with a mean age of 63.5 ± 7.2 years. The mean Simple Shoulder Test (SST) scores for the 27 culture-positive shoulders improved from 3.2 ± 2.8 points before the surgical procedure to 7.8 ± 3.3 points at a mean follow-up of 45.8 ± 11.7 months after the surgical procedure (p < 0.001), a mean improvement of 49% of the maximum possible improvement.
These authors point out that cultures taken at the time of revision shoulder arthroplasty are often positive for Propionibacterium. They tested the hypothesis that the functional outcomes of revising Propionibacterium culture-positive failed arthroplasties with a single-stage revision and immediate antibiotic therapy are not inferior to the clinical outcomes of revising failed shoulder arthroplasties that are not culture-positive.
Fifty-five shoulders without obvious clinical evidence of infection had a single-stage revision arthroplasty. Specifically all components (humeral and glenoid) were removed, a thorough debridement was carried out and a new humeral hemiarthroplasty was inserted with Vancomycin impregnated allograft. The residual glenoid bone was smoothed, but not bone grafted. No glenoid components were replaced.
After all culture specimens were obtained, 15 mg/kg of vancomycin and 2 g of ceftriaxone were administered intravenously. Patients were continued on antibiotics until the results of the cultures were finalized. Two or more cultures became positive, the infectious disease service started intravenous ceftriaxone and/or vancomycin through a PICC line with oral rifampin for 6 weeks followed by oral antibiotics in the form of amoxicillin and clavulanate or doxycycline for a minimum of 6months.
The patient self-assessed functional outcomes for those shoulders with ≥2 positive cultures for Propionibacterium (the culture-positive group) were compared with shoulders with no positive cultures or only 1 positive culture (the control group).
Below is an example of what is referred to as a 'stealth' presentation in which there were no preoperative symptoms or signs of infection, yet the cultures from revision surgery were strongly positive.
The culture-positive group were 89% male with a mean age of 63.5 ± 7.2 years. The mean Simple Shoulder Test (SST) scores for the 27 culture-positive shoulders improved from 3.2 ± 2.8 points before the surgical procedure to 7.8 ± 3.3 points at a mean follow-up of 45.8 ± 11.7 months after the surgical procedure (p < 0.001), a mean improvement of 49% of the maximum possible improvement.
The control group were 39% male with a mean age of 67.1 ± 8.1 years. The mean SST scores for the 28 control shoulders improved from 2.6 ± 1.9 points preoperatively to 6.1 ± 3.4 points postoperatively at a mean follow-up of 49.6 ± 11.8 months (p < 0.001), a mean improvement of 37% of the maximum possible improvement.
Subsequent procedures for persistent pain or stiffness were required in 3 patients (11%) in the culture-positive group and in 3 patients (11%) in the control group; none of the revisions were culture-positive.
The authors concluded that the clinical outcomes after single-stage revision for Propionibacterium culture-positive shoulders were at least as good as the outcomes in revision procedures for control shoulders. Two-stage revision procedures may not be necessary in the management of these cases.
Fourteen patients reported side effects to antibiotics, indication that patients should be educated with regard to potential antibiotic side effects.
===
We have a new set of shoulder youtubes about the shoulder, check them out at this link.
Be sure to visit "Ream and Run - the state of the art" regarding this radically conservative approach to shoulder arthritis at this link and this link
Use the "Search" box to the right to find other topics of interest to you.
You may be interested in some of our most visited web pages arthritis, total shoulder, ream and run, reverse total shoulder, CTA arthroplasty, and rotator cuff surgery as well as the 'ream and run essentials'