Evaluation of Clinical and Radiographic Outcomes After Total Shoulder Arthroplasty with Inset Trabecular Metal-Backed Glenoid
These authors assessed clinical and radiographic outcomes at midterm follow-up of anatomic total shoulder arthroplasty using a Zimmer Biomet trabecular metal glenoid component placed with full backside support using an inset technique. The glenoid components were used in a press-fit manner, which is "off label" in the U.S..
Of 39 patients who having 41 total shoulder arthroplasty procedures with the Zimmer glenoid component, 35 patients (37 shoulders) were available for a minimum 2 year (average 7.2 years, range, 2-11) clinical follow-up.
At final follow-up, the average shoulder elevation was 153 ± 22° and external rotation was 53 ± 12°. Average ASES scores were 86.8 ± 19.0, and VAS scores were 1.3 ± 2.4. Nine shoulders (27%) had metallic debris. Metal debris was not associated with inferior clinical outcomes.
However, the 39% of shoulders with radiolucencies around the glenoid had inferior clinical outcomes (due to the small number of cases, some of these differences are not statistically significant).
No patient had a reoperation.
Comment: This study of minimum 2 year results shows that good outcomes can be obtained with a trabecular metal glenoid component in type A glenoid pathology; this type of pathoanatomy is the most straightforward of all the glenoid types. The study does not provide data on the use of this implant for the more problematic glenoid types: B1, B2, B3, C, and D.
Even for the type A glenoids, the study does not provide evidence that the trabecular metal component is superior to the commonly used all-polyeythene component. For example, this study found a 39% rate of radiolucency, which is not lower than that reported for all-polyethylene glenoids (see this link).
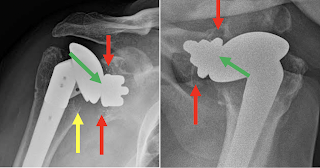
In one of the examples shown in the paper, there is a small amount of metal debris, but apparently secure component fixation with a substantial radiographic joint space (green arrows), centering of the humeral head in the glenoid and no evidence of osteolysis or stress shielding.
In the other illustrated case, the humeral head is superiorly decentered on the glenoid, no radiographic joint space is seen (green arrows) suggesting polyethylene wear, osteolysis around the glenoid (red arrows), and humeral osteolysis (yellow arrow). It is possible that the osteolysis resulted from polyethylene wear debris. Polyethylene wear has been recognized as an issue with metal backed components (see this
link).
A final issue with trabecular metal glenoid components is the difficulty of their removal, as may become indicated for infection or for conversion to a reverse total shoulder in the event of rotator cuff failure. Extraction of the trabecular metal leaves a substantial glenoid defect as well as posing a risk for fracture.
Here are the x-rays of a recent case that presented to us for evaluation - note the loosening of the glenoid component and the osteolysis.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Shoulder arthritis - what you need to know (see this link) Shoulder arthritis - x-ray appearance (see this link) The smooth and move for irreparable cuff tears (see this link) The total shoulder arthroplasty (see this link). The ream and run technique is shown in this link. The cuff tear arthropathy arthroplasty (see this link). The reverse total shoulder arthroplasty (see this link).
Shoulder rehabilitation exercises (see this link).
This is a non-commercial site, the purpose of which is education, consistent with "Fair Use" as defined in Title 17 of the U.S. Code.
Note that author has no financial relationships with any orthopaedic companies.